[PERSONAL]: AI Saved My Ass.
$50K Could Save Yours Too.
I’m participating in an AI-driven colon cancer prevention study — and helping to raise $50,000 to run it. 💰You can donate here. 🙏
Five years ago — and this is not an exaggeration — I wouldn’t have a colon right now, despite being in deep IBD remission for so long I can’t remember the last flare. If you had handed 2020-era gastroenterologists my chart — years of ulcerative colitis, chronic inflammation, prior high-grade dysplasia — the consensus would have been: colectomy. Take the colon out before the colon takes you out.
But medicine changes. And technology changes. And in IBD, we’re living through a quiet revolution in how precancerous lesions are found, understood, and managed. First chromoendoscopy; now AI. And I’m living proof of how much that matters.
I’m also now literally in an AI study aimed at preventing colon cancer in people like me — and I’m asking for your help to fund it. Let me explain why this is bigger than a “survey” and bigger than $50K.
Cancer Doesn’t Announce Itself
Ulcerative colitis and Crohn’s Disease (IBD) dramatically increases one’s lifetime risk of colon cancer. Not immediately or dramatically. But silently through years of inflammation, scar tissue, architectural distortion, and subtle dysplastic changes that don’t show up with neon arrows pointing to “THIS IS BAD.”
The hard truth: even the best GI doctors in the world can miss dysplasia. These lesions are often flat, pale, camouflaged, and shaped by scarred tissue that doesn’t behave like normal mucosa. This isn’t incompetence. This is the biology of chronic disease. For decades, many UC patients — including the version of me from five years ago — had one preventative option: remove the colon, the most aggressive procedure to avoid the worst outcome. And for many, that was the right decision.
But the tools have changed.
Chromoendoscopy: The First Leap That Bought Me Time
Chromoendoscopy is a technique where dye is sprayed through the colon to make subtle lesions visible. It changed the game by helping doctors detect flat dysplasia that white-light colonoscopy couldn’t see. You can read more about it in this 2016 press release about a long-term surveillance study led by my old doctor in NYC (James F. Marion, MD) that demonstrated chromoendoscopy’s superiority versus random biopsy or white-light for detecting dysplasia in patients with IBD.
It’s not an overstatement to say that chromoendoscopy is one of the reasons I still have my colon. It found what standard scopes might have missed. It allowed precise polyp and dysplasia removal and gave patients like me a fighting chance to stay under surveillance instead of under the knife.
But even chromoendoscopy has limits:
Dye only shows what’s visible.
Human eyes get tired.
Scarred tissue can hide lesions.
Subtlety still beats even the most experienced clinicians.
Which brings us to the next leap.
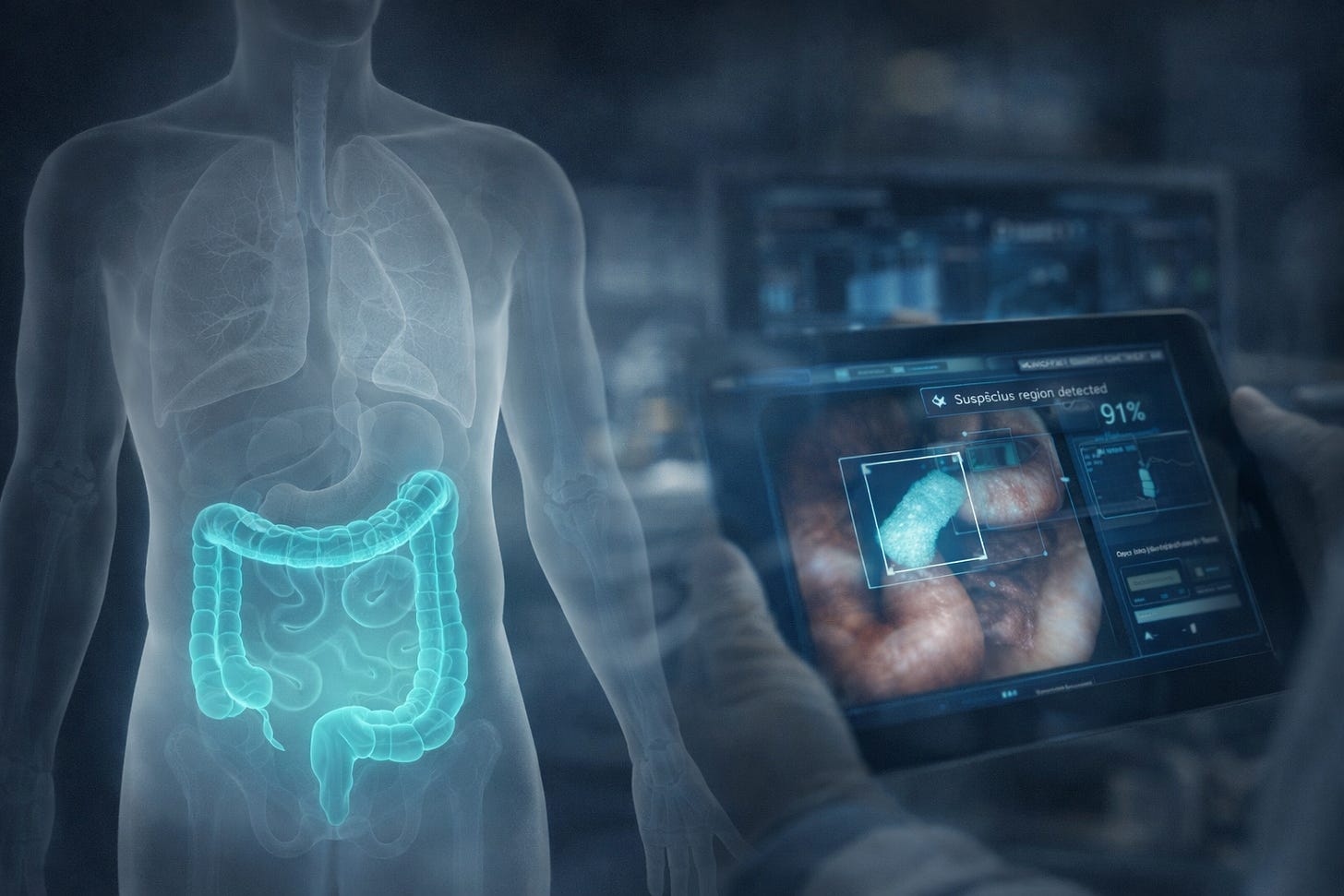
AI-Assisted Colonoscopy: The “Never Blinking” Second Pair of Eyes
This is the part most people don’t know yet: AI is already being used to detect colorectal polyps in real time. Europe and parts of Asia are ahead; and US adoption is growing quickly. The FDA has cleared multiple AI tools already that can:
Identify polyps the human eye misses.
Highlight suspicious areas in real time.
Reduce the rate of missed lesions.
Standardize detection across providers.
Improve outcomes especially in high-risk patients. (Hi. Remember me?)
For people with UC — people with scar tissue, architectural distortion, subtle dysplasia — AI isn’t optional. It’s the next critical safety layer. Because dysplasia in IBD isn’t a simple “polyp.” It’s often flat, irregular, and difficult to identify even for experts.
AI doesn’t get tired. It doesn’t blink. It doesn’t lose concentration at minute 47 of a long scope. It finds things and this technology is getting better fast. Watch the 6 second video above and you can see how Medtronic’s GI Genius identifies dysplasia in real time with a green box. (Not exactly the aforementioned neon arrows pointing to “THIS IS BAD,” but damn close enough.)
So the question is no longer: “Should AI be involved?” It’s: “How do we integrate it safely, ethically, and effectively for the people most at risk?” That’s what this study is actually about.
What the Study Aims to Do (and Why I’m In It)
This study / proposal, led by Dr. Loren Rabinowitz (my doctor and, no joke, former Olympic-caliber ice dancer ⛸️💃), is for a multi-center effort at Beth Israel Deaconess Medical Center focused on how AI-assisted colonoscopy can improve cancer prevention in ulcerative colitis. With $50,000 in support, the project examines both whether AI helps detect dysplasia earlier and how patients understand, trust, and experience AI-guided care — insights intended to inform national best practices.
This is not a study about whether patients are “OK” with AI. That’s far too simplistic. This is a study about how the next generation of cancer-prevention tools should be used:
How AI can support gastroenterologists in detecting dysplasia early.
How patients in the highest-risk categories understand and experience it.
How to design clinical workflows where humans and AI complement each other.
How to guide national best practices for AI-assisted colonoscopy.
How to bring chromoendoscopy-level advances into the AI era.
How to accelerate safer, earlier cancer prevention for UC patients everywhere.
This is the next version of the procedure I get every year or (usually) more — the one that may keep me alive. And yes, I’m participating because the stakes for people like me, and for my daughter, are enormous.
The Funding: $50,000 to Launch a Multi-Center Study That Moves This Forward
This funding is for the unglamorous, essential work that determines whether AI actually improves care. Here’s what the $50k actually pays for:
Survey and instrument design to capture patient experience without bias.
Pilot testing (because bad survey design = bad science).
Multi-center collaboration between BIDMC and Lahey to ensure strong patient diversity.
Research coordination, data collection, and analysis.
Publication and dissemination so the findings actually shape national practice.
It’s a one-year, high-impact, shovel-ready project with immediate output; i.e., not a forever fund. $50k effectively accelerates an entire area of IBD cancer prevention research.
Why I’m Asking For Help
First, last year made the stakes very real for me (again). TLDR all good, but: April findings raised concerns about low-grade dysplasia and triggered an initial surgery consult. It was wait and see until an October colonoscopy found and removed multiple polyps, but a subtle cecal lesion remained (see below - I blissfully blurred most of it for you - you’re welcome). This kept that surgery conversation alive (and my colon in jeopardy). If you didn’t hear from me much toward the end of last year, it’s because in December I underwent a successful “specialized / mini surgical” colonoscopy with an endoscopic mucosal resection performed by Dr. Tyler Berzin. That and a pristine pathology report afterward finally took (near term) surgery off the table (again / for now). That experience drove home how much depends on seeing the right things, at the right time, with the right tools.
But why else am I helping…?
Because this technology could save lives.
Because early detection is everything.
Because I’ve lived in the before-times — when missing a lesion could mean losing your colon.
Because even in 100% clinical remission, people like me still carry the scars of chronic inflammation and the risks that come with them.
Because my daughter has Crohn’s; and because the thought of her someday needing surveillance scares me — and I want her world to have every tool available.
Because these advances don’t happen on their own. They happen when people fund them.
If you’ve followed my writing on IBD, or my daughter’s story, or our Take Steps involvement — this is the next chapter. And I’m asking, sincerely, if you’ll help. Any amount supports this. $100. $250. $1,000. Whatever feels right.
Here is where you can donate directly.
Hope, But Earned
I never imagined I’d be in an AI study about colon cancer prevention. But here we are — and honestly, I’m grateful:
For the tools that kept me from surgery.
For the technology that’s arriving just in time for the next generation of patients.
For the doctors pushing this forward.
And I’m grateful for you for even reading this.
Chromoendoscopy changed what was possible. AI will change it again — for me, for my daughter, for thousands of families. Thank you for helping us get there.
PS - My Throne Science toilet camera that I wrote about here is en route. I got so excited to poop that I invested in their seed round 🚽🎥💩💰😊





The chromoendoscopy-to-AI progression here is fascinating because it shows how medical tech advances in layers rather than jumps. The fact that AI doesn't fatigue at minute 47 addresses something most people don't think about but makes total sense. My uncle had a similar IBD situation and the standard advice back then was pretty binary, either surveillance works or take the colon. Seeing how AI can spot flat dysplasias that even dye-enhanced scopes might miss feels like it fundamentaly changes the risk calculation for high-risk patients.